Deep Vein Thrombosis (DVT): Symptoms, Causes & Treatments
Imagine sitting through a long flight, feeling fine at first, but your leg begins to ache and swell later. This seemingly minor discomfort could be deep vein thrombosis (DVT).
DVT ranks as the third most common cause of “death from cardiovascular disease”, following heart attacks and strokes.
Often misunderstood and overlooked, DVT is more than just a blood clot. Understanding its risks, symptoms, and prevention can make all the difference.
What Is DVT?
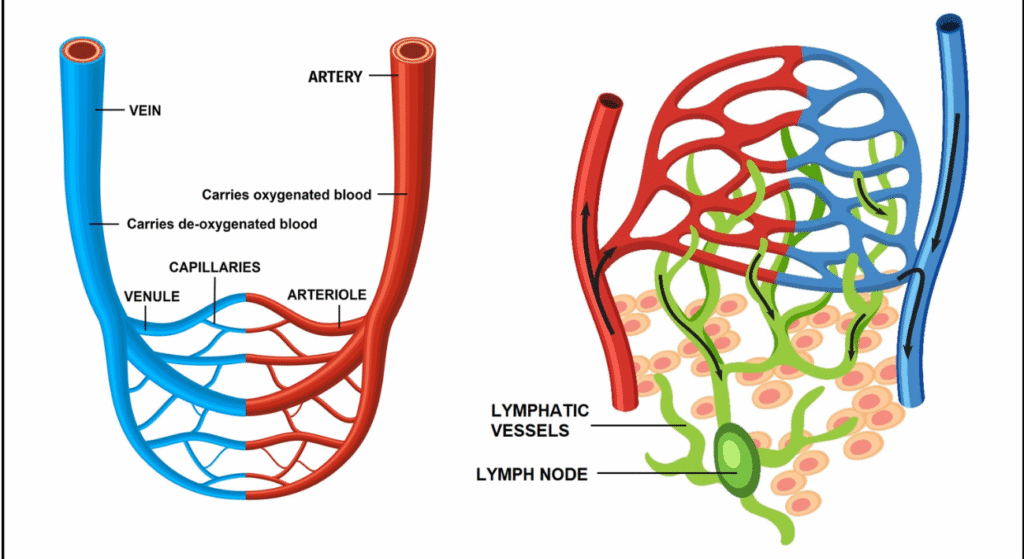
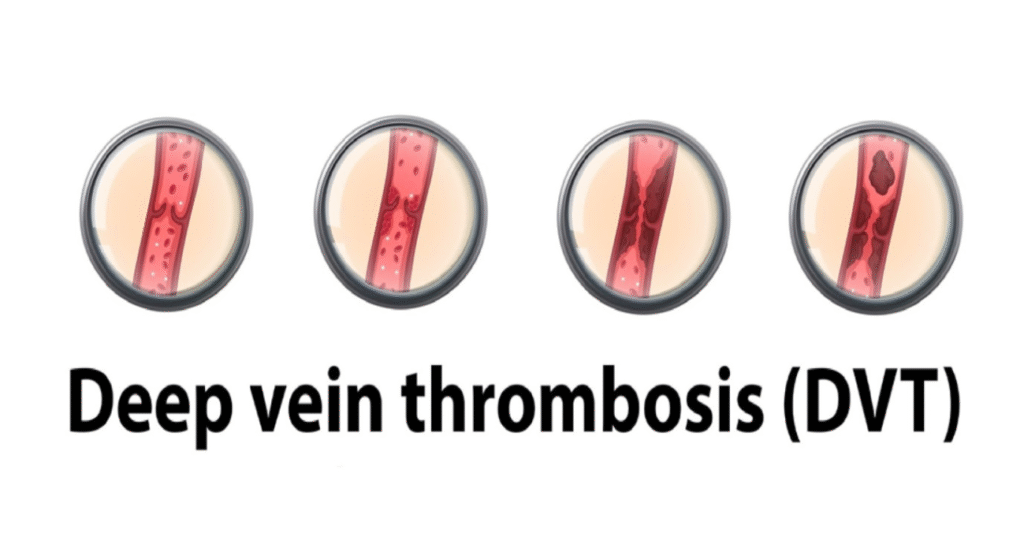
Deep vein thrombosis (DVT) is a blood clot that forms in the deep veins, typically in the arms or legs.
If left untreated, it can result in life-threatening complications like pulmonary embolism (PE).
Causes of DVT
DVT forms due to abnormal blood flow, vessel injury, or increased clotting. Common causes include:
- Immobility: Prolonged bed rest or long flights reduce blood flow.
- Pressure in Veins: Pregnancy, high BP or tumours can impede venous return.
- Venous Injury: Trauma or surgeries can damage veins.
- Increased Coagulation Risk: Conditions like cancer or genetic clotting disorders increase clot formation.
DVT Risk factors:
DVT risk factors are categorised as inherited or acquired.
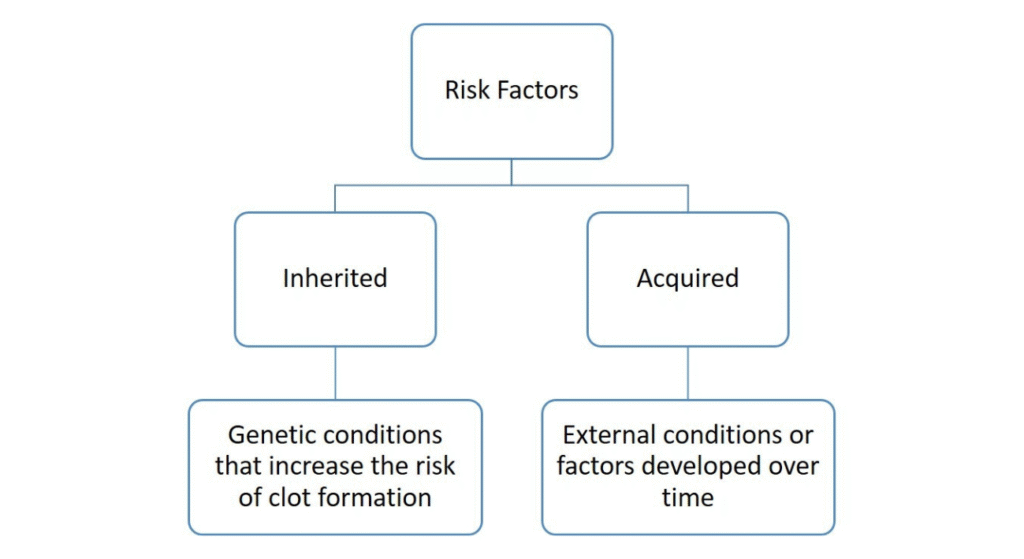
Inherited Risk Factors
Genetic conditions that cause hypercoagulability significantly contribute to DVT, including gene mutations and protein deficiencies. Some of these are:
- Prothrombin gene mutation: Increases clotting protein levels in the blood.
- Protein S deficiency: Shortage of a specific protein needed to stop clotting.
- Antithrombin deficiency: Not enough of a natural blood thinner.
- Non-O blood group: Blood types other than O increase clot risk slightly.
Acquired Risk Factors
Acquired risk factors are external conditions or lifestyle factors developed over time that increase the risk of DVT.
Acquired risk factors account for over 50% of cases and often overlap with hereditary factors.
- Surgeries, Trauma, and Immobilization: Major surgeries with long recovery periods increase the risk of clot formation.
- Cancer: Tumor-related hypercoagulability and cancer treatments, like chemotherapy or central venous catheters, raise the risk.
- Chronic Illnesses: Conditions such as heart failure, chronic kidney disease, inflammatory bowel disease, and lupus are linked to higher clotting risks.
- Pregnancy: The postpartum period increases clotting risk, with additional risk from obesity, advanced age, and hypertension.
- Lifestyle Factors: Smoking, obesity, and prolonged sedentary periods (e.g., long flights) increase DVT risk.
- Medications: Drugs like oral contraceptives, hormone replacement therapy, and certain cancer treatments elevate the risk of clot formation.
- Previous Thromboembolism: A history of clot & dislodgement events significantly increases the risk of recurrence, especially when combined with genetic factors.
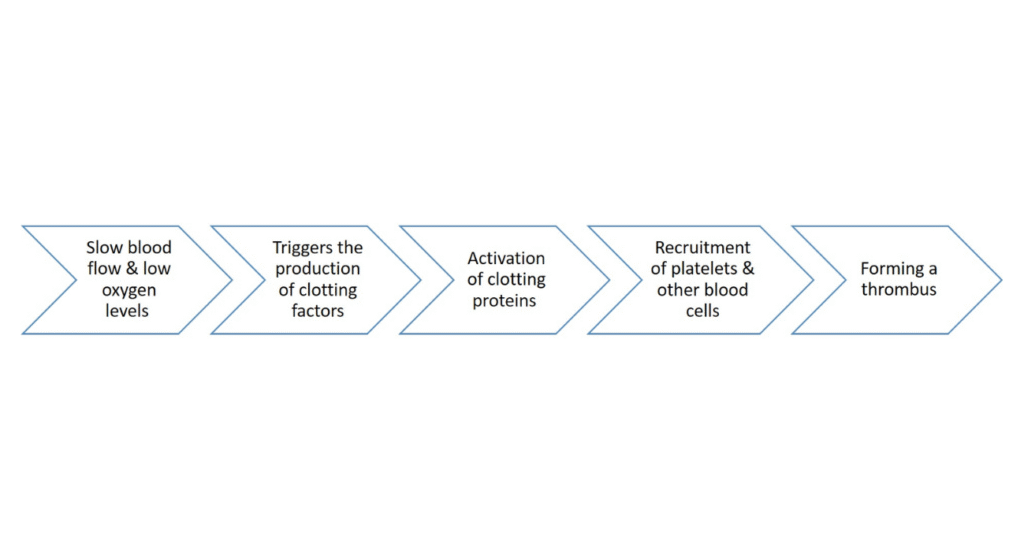
How DVT Develops?
The development of Deep Vein Thrombosis (DVT) is primarily driven by the mechanisms outlined in Virchow’s Triad.
These factors trigger normal clot formation as a natural response to seal damaged blood vessels. However, when the balance between clot formation and breakdown (fibrinolysis) is disrupted, DVT occurs.
- Venous stasis happens when blood flow becomes sluggish, especially near the valves in your legs. This is common during long periods of immobility.
- Vascular injury can occur from trauma or damage to blood vessel walls, triggering clot formation at the injury site.
- Hypercoagulability means your blood is more likely to clot. This can be caused by inherited genetic conditions or acquired factors.
Thrombus formation often begins at sites of venous stasis, like the calf veins in the leg or areas near venous valves.
Symptoms of DVT
The symptoms of acute lower extremity DVT vary depending on where the clot is, how large it is, and how much of the blood vessel is blocked. Symptoms are non-specific & range from mild to severe.
Up to 50% of patients with acute DVT may not have any specific signs or symptoms.
Common Symptoms:
- Pain in the calf
- Swelling (oedema)
- Redness (erythema)
- Tenderness to touch
- Fever
- Visible veins near the surface of the skin
- Pain with foot movement Cyanosis (bluish discolouration) in the affected area.
A rare and severe form of DVT is seen with a triad of:
- Massive swelling
- Cyanosis
- Pain
This happens when the blood outflow in a limb is completely blocked, causing pressure buildup, thus increasing the risk of tissue death called gangrene.
DVT symptoms are often mistaken for other conditions, such as lymphedema or cellulitis. If you experience any of these symptoms, seek medical attention immediately to avoid serious complications of vein thrombosis.
Diagnosis of DVT
Diagnosis of DVT involves a combination of clinical evaluation and diagnostic tests to confirm the presence of a blood clot in vein.
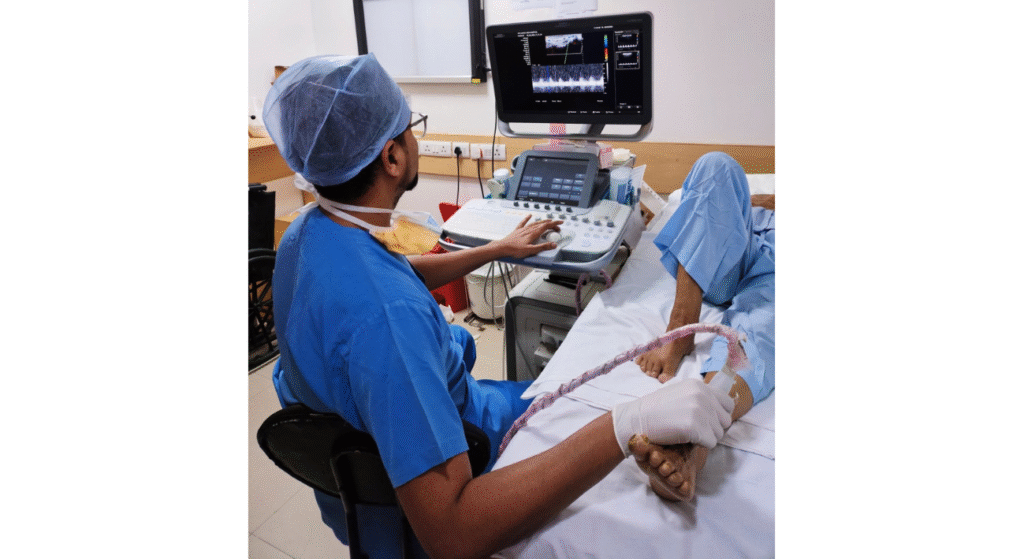
Ultrasound:
The primary test for diagnosing DVT is a Duplex ultrasound. However, CT venography is considered the gold standard for diagnosis.
D-dimer Test:
If the ultrasound is negative but symptoms still suggest DVT, a D-dimer blood test may be done to check for substances released when a clot breaks down.
Prevention of Deep Vein Thrombosis
Simple lifestyle changes can reduce your risk of developing a blood clot in the leg vein:
- Move around: Avoid sitting still for long periods. Flex your ankles or take short walks when driving or flying.
- Exercise: Aim for at least 30 minutes of moderate activity daily.
- Stay hydrated: Drink plenty of water to improve circulation.
- Quit smoking: Smoking raises DVT risk, so quitting helps circulation.
- Maintain a healthy weight: This lowers the risk of DVT.
- Wear compression stockings: For those at risk, these help prevent DVT by improving blood flow.
- Follow medication advice: Take prescribed blood thinners as suggested by the vascular specialist.
Treatment for DVT
The goal of DVT treatment is to prevent the clot from growing and to reduce the risk of complications, such as pulmonary embolism (PE). The primary treatment methods include anticoagulants and, in some cases, endovascular interventions.
Anticoagulants:
- Vitamin K antagonists (VKAs): Typically prescribed for 3 months to prevent the clot from growing and to avoid new clots from forming.
- Direct oral anticoagulants (DOACs): These offer an alternative to VKAs, with easier management and fewer monitoring requirements.
Endovascular Interventions:
- Catheter-directed thrombectomy: A procedure to remove large clots directly from the veins.
- Stenting: Used in some cases to keep blood vessels open after clot removal.
- Mechanical thrombectomy: Involves using devices to physically remove or break down the clot.
- Inferior vena cava (IVC) Filter: If you can’t take anticoagulants due to high bleeding risk, a doctor may place an IVC filter to prevent clots from travelling to the lungs and causing PE.
Compression Stockings: To reduce swelling and pain, graduated compression stockings may be recommended. They help improve blood flow and prevent complications.
Treatment duration and methods vary depending on the patient’s specific condition and response to therapy. Always consult with a qualified vascular surgeon to determine the best treatment plan for your condition.
FAQs
Can DVT Be Cured?
Yes, deep vein thrombosis (DVT) can be treated and managed effectively. Treatment options vary based on the clot’s severity and individual factors. These include:
- Blood thinners: To prevent further clot formation and help dissolve the existing clot.
- DVT thrombolysis: A procedure to dissolve the clot using medication.
- Surgery: In severe cases, to remove the clot or address complications.
- Compression socks: To reduce swelling and improve circulation.
- Leg elevation: To decrease swelling and enhance blood flow.
While most patients recover completely, some may experience long-term symptoms such as leg pain or swelling. Preventive steps, like avoiding prolonged immobility, prevent future clots. Early treatment gives the best chances for full recovery.
Is DVT Life-Threatening?
Yes, deep vein thrombosis (DVT) can be life-threatening if left untreated. The risks include:
Pulmonary Embolism (PE): A clot can break free from the vein and travel to the lungs, causing a pulmonary embolism. PE is a medical emergency and can be fatal. Symptoms include:
- Sudden shortness of breath
- Chest pain
- Rapid breathing
- Coughing up blood
Post-Thrombotic Syndrome: Even after the clot dissolves, damage to the veins may cause long-term issues like:
- Pain
- Swelling
- Skin discoloration
- Leg ulcers
Starting treatment within 14 days is crucial for best results and without complications.
How to Check for DVT at Home?
To check for DVT at home, follow these steps:
- Look for Swelling: Compare the size of your legs. Notice any unusual swelling in one leg.
- Check for Pain: Gently press along your leg. Pain or tenderness may indicate a clot.
- Assess Skin Color: Observe your legs for redness or any unusual discolouration.
- Feel for Warmth: Touch your legs. Areas that feel warmer than usual could signal DVT.
While these checks can help, only a vascular specialist can confirm the diagnosis. If you notice these signs, contact a vascular surgeon near you immediately.
Take Home Message
Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in the veins, typically in the legs, due to abnormal blood flow, vessel injury, or increased clotting. The severity of the condition tends to increase when the clot is located higher up in the leg.
Simple lifestyle changes can help reduce the risk of DVT. Consulting a vascular surgeon for proper management is essential in preventing complications and ensuring the best outcomes.
Don’t let fear hold you back—consult a vascular expert today!
We hope this blog answers your concerns about DVT treatment and prevention! Have more questions or topics you’d like us to cover? Drop a comment or send us a DM!
Stay tuned for next week’s blog!