What Are Varicose Veins?
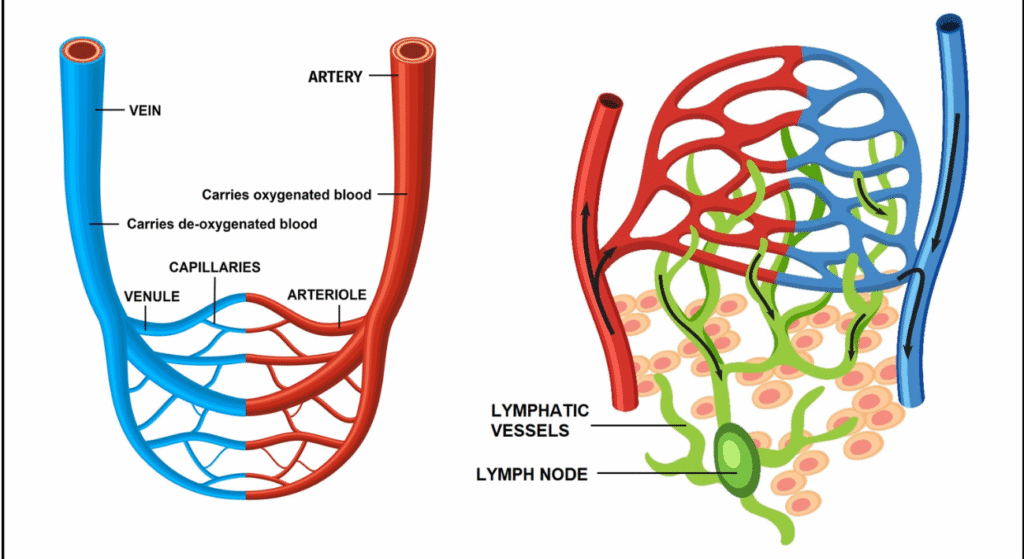
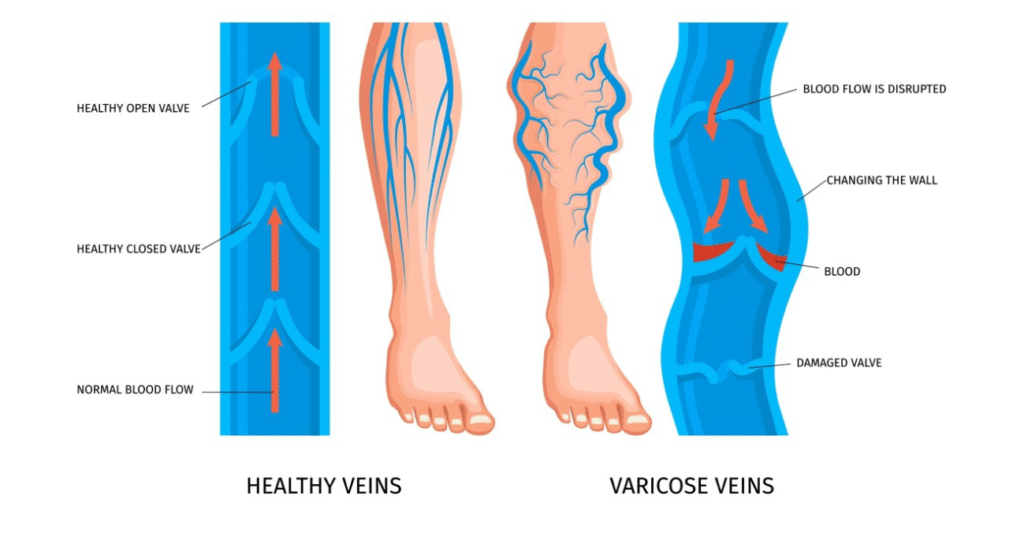
Varicose veins in the legs are swollen and tortuous superficial veins visible beneath the skin. They result from faulty valves in the veins, which prevent blood from flowing efficiently.
What Causes Varicose Veins in Legs?
Varicose veins occur when vein walls weaken, and valves fail to send blood back to the heart as efficiently as they normally would. As a result, blood pools in the veins, causing them to enlarge.
Risk Factors
Certain factors increase the likelihood of developing varicose veins. Understanding these can help identify high-risk individuals and practice preventive measures. These include:
- Family History: Genetic predisposition is the most significant risk factor due to inherited traits that weaken vein walls or valves.
- Age: Aging weakens vein walls and valves, making older individuals more prone to varicose veins.
- Gender: Women are more prone to varicose veins due to hormonal fluctuations. Estrogen and progesterone can relax vein walls, impairing their ability to push blood back to the heart effectively.
- Occupation: Prolonged standing in jobs strains the leg veins, heightening the risk.
Talk about occupational risk—vascular surgeons often find themselves battling the very varicose veins they treat!
- Constipation: Straining raises abdominal pressure, impairing blood flow and increasing the likelihood of varicose veins.
- Smoking: Damages blood vessels, weakens vein walls, and aggravates venous insufficiency.
- Pregnancy: Increased blood volume and hormonal changes weaken veins. Multiple pregnancies further elevate the risk.
- Hormonal Therapy: Treatments like HRT relax vein walls, mimicking the effects of natural hormonal fluctuations.
- Diabetes: High blood sugar damages veins, reducing elasticity and blood flow efficiency.
- Hypertension: Elevated pressure stresses vein walls, causing them to expand and form varicose veins.
- Venous Thrombosis History: Blood clots can damage valves, disrupting normal blood flow and predisposing to varicose veins.
- Leg Trauma: Injuries can damage veins, leading to impaired blood flow and varicose veins.
Stages of Varicose Veins
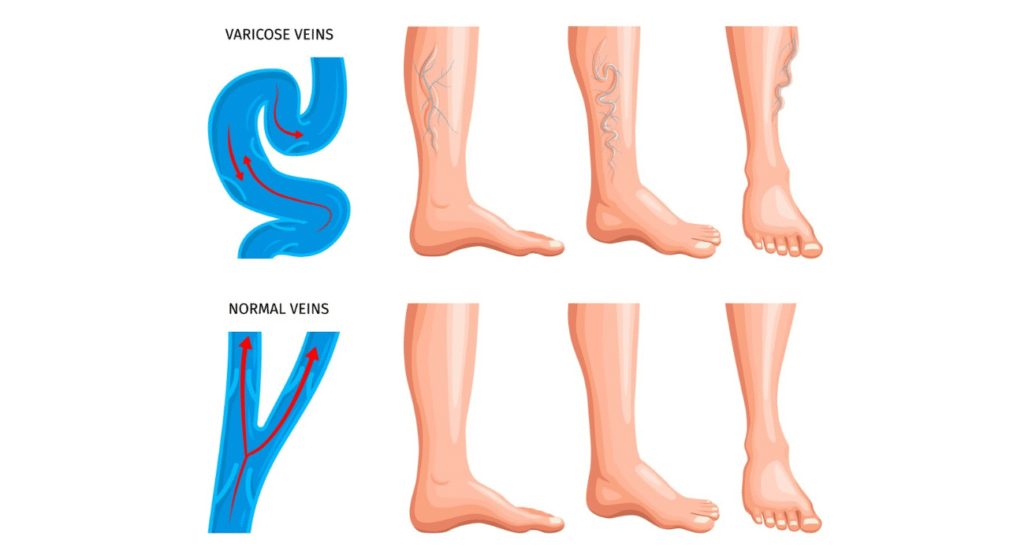
Varicose veins progress through several stages:
Stage 1 (Spider Veins): Tiny, visible veins with no symptoms.
Stage 2: Enlarged, bulging (varicose) veins noticeable under the skin.
Stage 3: Swelling in legs and ankles due to fluid retention.
Stage 4: Skin pigmentation and hardening around the veins.
Stage 5-6: Non-healing, long-standing ulcers and complications like bleeding.

Varicose Veins Symptoms
Varicose veins can cause various symptoms, ranging from mild discomfort to significant physical changes. The most common ones are:
- Leg heaviness and fatigue: A persistent feeling of weight and tiredness in the legs.
- Dull-aching Pain: Discomfort that worsens after standing or sitting for long periods.
- Itching: Irritation around the affected veins, often leading to scratching.
- Cramps: Night-time leg cramps that disturb sleep.
- Mild tenderness: Sensitivity around swollen veins.
- Skin discoloration: Darkening of the skin, usually around the ankle and calf.
- Exercise intolerance: Difficulty engaging in physical activity due to leg discomfort.
- Visible changes: Distended veins that appear twisted, often running from the thigh to the ankle.
- Long-standing ulcer: Chronic, non-healing, painful ulcer(s), particularly around the ankle region.
Preventive Measures for Varicose Veins
Although complete prevention of varicose veins may not always be possible, some steps can help reduce the risk and alleviate symptoms:
- Wear Compression Stockings: These specially designed stockings apply gentle pressure to your legs, supporting veins and improving blood flow. They can reduce swelling and provide relief to those who stand or sit for extended periods.
- Elevate Your Legs: Periodically lifting your legs above heart level allows gravity to assist in blood flow back to the heart, reducing the pooling of blood in the veins. This is especially helpful after a long day on your feet.
- Incorporate Regular Exercise: Physical activities like walking, swimming, or cycling help strengthen leg muscles, which act as natural pumps for your veins. Stronger muscles promote better blood flow and reduce the strain on veins.
- Avoid Prolonged Standing or Sitting: Staying in one position for too long can slow blood circulation. Shift positions regularly, take short walks, or flex your legs to encourage blood flow.
Diagnosis of Varicose Veins
The gold standard for diagnosing varicose veins is a duplex ultrasound (DUS), a non-invasive test that evaluates vein structure and blood flow. Additional methods, such as medical history, physical examination, and venography, serve as adjuncts for a comprehensive assessment.
Duplex Ultrasound: The Gold Standard
The duplex ultrasound (DUS) also called Doppler, is a painless and non-invasive imaging test using sound waves to visualise veins and assess blood flow.
- How it works: A technician applies warm gel to the legs and uses a handheld device (called a transducer) to transmit sound waves, creating real-time images of blood vessels on a monitor.
- What it shows: Documents vein patency or opening, valve competency, vein diameters and locations of abnormalities.
- Duration: Painless and takes 15-20 minutes per leg.

Varicose Veins Treatment
Modern treatment options range from conservative to surgical approaches, depending on the severity of the condition:
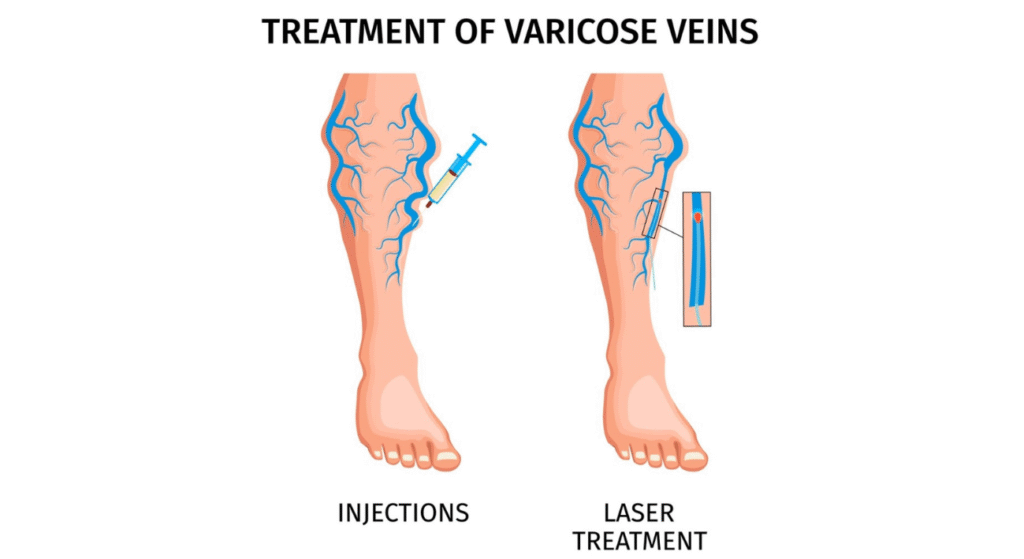
Minimally-Invasive Treatment:
- Sclerotherapy: A solution is injected into the veins, causing them to close up and eventually fade.
- Laser therapy for varicose veins: A laser is used to heat and seal off the problematic veins, making them disappear over time without incisions.
- Endovenous Laser Ablation (EVLA): A more advanced version of laser therapy that uses heat to treat veins from the inside.
- Endovenous Radiofrequency Ablation (RFA): Heat generated by radiofrequency energy is used to close off and shrink damaged veins.
- Endovenous Glue Ablation (VenaSealTM): A medical adhesive is injected into the vein to seal it shut, allowing blood to reroute through healthier
Surgical Treatments:
- Venous Ligation: A surgical procedure where the affected vein is tied off to prevent blood flow, often combined with vein removal for severe cases.
- Microavulsions: Small incisions are made to remove the varicose veins from the skin surface.
- Vein stripping: A surgical procedure where large varicose veins are removed from the body. This is performed in extreme situations and is otherwise obsolete today.
This is a simplified overview of treatment options for varicose veins, intended to give a basic understanding of the available approaches. For more details on the specific procedures and protocols, consult a qualified vascular surgeon near you.
Take-Home Message
Varicose veins can significantly impact daily life, but effective treatments exist. They cannot be entirely stopped or reversed, but their progression can be delayed. Regular exercise, a healthy diet, and wearing compression stockings improve circulation. Certain home remedies can help to manage symptoms like pain-relieving creams or tablets.
While other specialists offer alternatives, the expertise of vascular surgeons in managing varicose veins is unparalleled. Trust your care to the true specialists.
FAQs
What Causes Varicose Veins in the Scrotum?
Varicocele, or varicose veins in the scrotum, occurs due to malfunctioning valves in the veins of the testes called spermatic veins. This condition is more common in young men and may lead to infertility if untreated. Vascular surgeons often recommend minimally invasive treatments for symptomatic cases.
Varicose veins can also develop in other areas, such as the rectal region, where they are known as haemorrhoids or piles. A proctologist, a specialist in treating conditions of the rectum and anus, typically manages this condition.
Can You Stop Varicose Veins?
No, varicose veins cannot be entirely stopped or reversed, but their progression can be delayed. Regular exercise, a healthy diet, and wearing compression stockings can help improve circulation. Early consultation with a vascular surgeon is important for managing symptoms effectively.
Additional Tips to Delay Progression:
- Maintain a healthy weight.
- Avoid prolonged sitting or standing; try to move every 30 minutes.
- Avoid prolonged time in the washroom
- Elevate your legs to reduce pressure in veins; raise your feet above the heart level several times a day – especially at bedtime.
- Avoid high heels for prolonged periods.
- Wear compression stockings.
- Eat a healthy diet rich in fibre and low in salt.
- Quit smoking to reduce vein damage.
- Avoid tight clothing.
How To Remove Varicose Veins at Home?
Home remedies cannot remove varicose veins but can help to manage symptoms:
- Walking: Improves circulation.
- Hydration: Drinking water supports vein health.
- Exercise: Low-impact activities strengthen leg muscles.
- Massage: Helps reduce swelling, but you must avoid direct pressure on veins.
For permanent removal, treatments like laser therapy or surgery are necessary.
What Is Laser Treatment for Varicose Veins?
Laser treatment for varicose veins is a minimally invasive procedure that uses laser energy to treat damaged veins. It is considered effective, safe, and often preferred over traditional surgery for its quick recovery.
Here’s some more information about it:
- Procedure: A catheter is inserted into the vein, and laser energy is used to heat and collapse the vein walls.
- Benefits: The closed veins are eventually absorbed by the body, resulting in improved blood flow and reducing the appearance of varicose veins.
- Minimally invasive: The procedure is performed under regional anaesthesia and typically has minimal downtime.
- Recovery: Most patients resume daily activities within a day.
Don’t linger on the throne—your veins will thank you for the quick exit!
I hope this blog answers most of your questions! Let us know what topics you’d like us to cover next—drop a comment or DM us.
Stay tuned for our next blog!